Children’s Hospitals
Health Care Landscape
Service Lines
The Impact of Abortion Bans on Neonatal Intensive Care Utilization: An Analysis Leveraging the Vizient® Clinical Data Base
Editor's note: Hannah Murphy, Lead, Analytics & Insights also contributed to this blog post.
Welcome to the Pediatric Research at Vizient blog series. This series highlights some of our latest findings in pediatric medicine and incorporates analysis leveraging the Vizient® Clinical Data Base to support our pediatric research efforts. If you haven’t already, check out the first and second blog posts in our series.
In this third post of our series, we provide insights from Vizient research on changes in neonatal intensive care unit (NICU) utilization and outcomes following the implementation of restrictive abortion policies, findings from which were presented at the American Academy of Pediatrics National Conference and Exhibition in September 2025.
State-level abortion policies changed dramatically following the US Supreme Court’s decision in Dobbs v Jackson Women’s Health Organization in June 2022 when several states immediately imposed complete or six-week abortion bans. Studies show subsequent rises in fertility rates, infant mortality rates and congenital anomaly incidence in states with restrictive abortion policies.
The current study aimed to assess the impact of such policies on NICU demand and outcomes by examining the portion of births admitted to the ICU, and among births with ICU utilization: ICU length of stay, total length of stay, and in-hospital mortality. We compared these outcomes in states with restrictive abortion policies to those without, using a “pre-ban” timeframe of 2019 to 2022 and an “under ban” timeframe from 2023 to 2024.
We analyzed 6,205,325 births from 2019 to 2024, representing 28% of total US births. This included 1,302,984 births from 129 hospitals in “ban” states, and 4,902,341 births from 469 hospitals in “no ban” states.
Our findings highlight increased NICU demand in states that have imposed restrictive abortion policies that will need to be addressed by increased bed and workforce capacity. The following results pertain to the neonatal population studied.
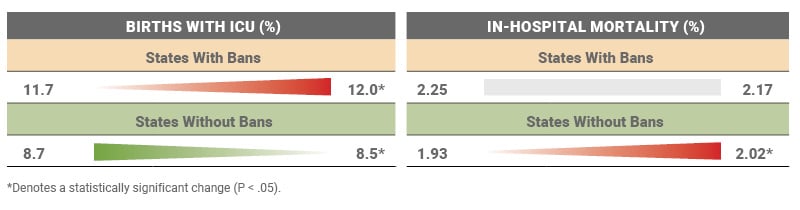
Key Finding #1: NICU Utilization Increased in States That Implemented Total or Six-Week Abortion Bans
In states with bans, the portion of births admitted to the ICU, the ICU length of stay, and the total length of stay is higher under ban than before the ban. In states without bans, the portion of births admitted to the ICU and the total length of stay decreased during the same time period.
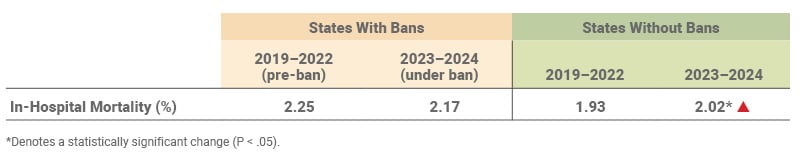
Key Finding #2: In-Hospital Mortality Rate Did Not Change Following the Implementation of a Ban
In states with bans, in-hospital mortality declined modestly and without statistical significance from 2.25% pre-ban to 2.17% under ban. Interestingly, in-hospital mortality did increase in the group of states without bans from 1.93% to 2.02%. Important to note, in-hospital mortality only reflects mortality during the hospital stay and does not capture neonatal (28 days) or infant (one year) mortality.
Key Finding #3: Ban States and Non-Ban States Differed Significantly Prior to Dobbs
NICU admission rate and in-hospital mortality were higher in ban states than non-ban states pre-Dobbs, indicating baseline differences in the two groups. Post-Dobbs, the NICU admission rate further widened while the in-hospital mortality gap narrowed.
Sg2 Perspective
These findings add the hospital-based perspective to the growing body of literature analyzing the impact of a more fragmented abortion policy landscape following the 2022 Dobbs decision. Taken together, these data-driven insights support proactive management of neonatal intensive care and inform strategic planning efforts for this priority service area.
Hospital leaders in states with restrictive abortion policies must:
- Anticipate rising capacity and workforce constraints. Monitor changes in neonatal case mix and ICU demand and leverage these data points to advocate for more resources or modification of care and/or referral pathways.
- Enhance partnerships that support acute care operations and upstream care delivery. Deepen perinatal regionalization efforts that seek to align maternal and neonatal acuity with hospital level of care. Also consider partnering in neighboring states for support with access, workforce training and capacity management.
- Layer in local and community-based nuances. Consider market-specific dynamics in your strategic approach, like proximity to out-of-state reproductive health care, social barriers and disproportionate access, state-specific ban policy, market population shifts, and more.
Click here to access the full research presentation on this topic.
Note: The 14 “ban states” include Alabama, Arkansas, Georgia, Idaho, Kentucky, Louisiana, Mississippi, Missouri, Oklahoma, South Dakota, Tennessee, Texas, West Virginia and Wisconsin. Sources: Bell SO et al. JAMA. 2025;333(15):1324–1332; Gemmill A et al. JAMA. 2025;333;(15):1315–1323; Tseng SY et al. Pediatr Open Sci. 2025;1(3):1–8; Vizient Clinical Data Base. Irving, TX: Vizient, Inc.; 2025. https://www.vizientinc.com.